For families of children with disabilities and chronic conditions, Medicaid isn’t just insurance — it’s a lifeline.
Medicaid provides therapies, in-home nursing, medical equipment, and treatments that allow children with special health care needs (CSHCN) to live, learn, and thrive. And unlike employer-based insurance, which often excludes or limits pediatric therapies, Medicaid guarantees comprehensive, continuous care tailored to children’s evolving medical needs.
Unfortunately, Congress is threatening this lifeline by proposing $880 billion in cuts to the Medicaid program, which puts at risk the health coverage of the 37 million children who rely on Medicaid for their health coverage. If Medicaid is cut, capped, or restricted, children with special health care needs would be disproportionately harmed.
Rolla Sweis, president and CEO at La Rabida Children’s Hospital and Dr. Jon Rodasta, chief medical officer at University of Illinois Health, both explain how such cuts would be devastating to children and health providers in this video.
Such a radical change is reminiscent of the Trump Administration’s proposal in 2017 to “repeal and replace” the Affordable Care Act (ACA) and to slash Medicaid by more than $800 billion.
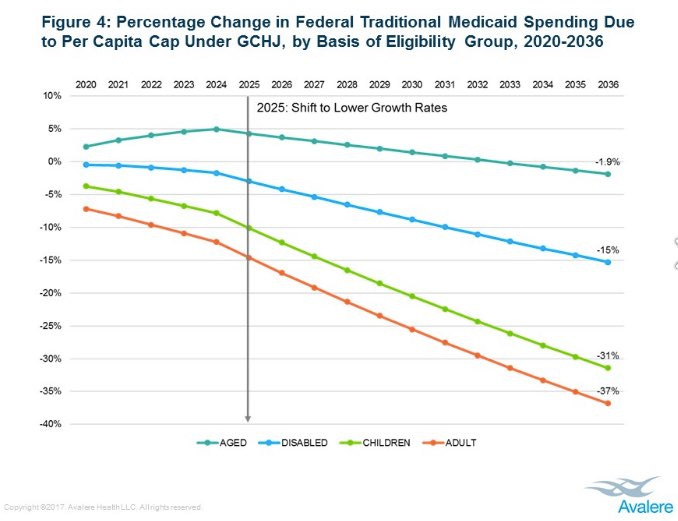
A study by Avalere Health of the Senate version of the bill found that it would have disproportionately impacted children’s health, cutting their Medicaid funding by an astounding 31%.
A Medicaid per capita cap would subject states to arbitrary limits on how much the federal government would contribute per enrollee, regardless of actual costs or medical needs. This arbitrary limit would force states to deny coverage, ration care, and reduce services – hitting children with the most serious health conditions the hardest.
Who Would Be Harmed?
In making their case to slash funding, House Republican leadership has argued the resolution never explicitly mentions Medicaid for cuts but directs the House Energy and Committee Committee to make $880 billion in cuts.
If Medicare is exempt from the cuts, the Congressional Budget Office (CBO) recently confirmed, that 93% of what is available for the House Energy and Commerce Committee to cut would be from Medicaid. That figure is 96% when the Children’s Health Insurance Program (CHIP) is factored in.
In other words, the bulk of cuts would likely be imposed upon Medicaid and/or CHIP and likely target children.
Those with higher costs, such as children with special health care needs, would be at greatest risk. The reason is that a per capita cap would establish a rigid funding amount per child, person with disabilities, senior citizens, and low-income adult.
States would be forced to “save money” by:
Denying coverage or care to children with the most expensive health conditions, such as cancer.
Reducing benefits like in-home care and life-saving treatments, forcing parents to choose between work and caregiving.
Delaying or cutting access to specialists and critical therapies for kids with autism, Down syndrome, cerebral palsy, etc.
For example, if a per capita cap or limit of $3,000 per child is imposed on a state, but a child with cancer requires nearly $400,000 in treatment, states would have an immense financial incentive to deny or limit care.
With Medicaid’s federal-state matching system or FMAP (federal medical assistance percentage), a state with a 60/40 match would be left covering everything above $1,800 per child, which is a monumental financial burden that could force severe rationing of care.
Realities of Managed Care
Health plans already have incentives to limit care for high-cost cases, and Medicaid managed care has inherent problems when it comes to serving children with special health care needs. According to a report to Medicaid and CHIP Payment and Access Commission (MACPAC) entitled “Access to Care for Children with Special Health Care Needs: The Role of Medicaid Managed Care Contracts” by Health Management Associates and the Urban Institute:
…capitated managed care organizations have a financial incentive to control utilization, which could result in barriers to access to certain health care providers and services; [managed care organizations] MCOs may have inadequate provider networks and/or insufficient accommodations for ongoing or very specialized care needs; some MCOs may not have deep experience serving children with a wide array of medical, developmental, emotional, and/or behavioral issues….
A separate study found that increased Medicaid managed care (MMC) enrollment was “associated with less access to specialties like [mental health] MH and increased frustrations among caregivers seeking services for their children.”
To protect the health of CSHCN, Medicaid agencies need to have contract standards that promote the delivery and access to medical care and services. As an example, federal rules require managed care plans to provide direct access to specialists (see 42 C.F.R. § 438.208(c)(4)) through “standing referral or an approved number of visits” for “enrollees with special health care needs.”
These contract standards are far from perfect and should be improved, but in a world of Medicaid caps or limits, both states and the federal government would have an increased financial incentive to deny, limit, and ration care and services to kids, particularly children with special health care needs, rather than protect them.
Under the current needs-based funding structure, the federal government’s match helps ensure that children receive the care they need, such as for advances in medical treatment, and through economic downturns, inflation, natural disasters, an epidemic, etc. In the last few years, we have witnessed all of these things and should ensure Medicaid remains flexible to account for changing circumstances.
Unfortunately, a per capita cap would gut this flexibility, locking in permanent underfunding that worsens over time and becomes tragic at those moments when children need the most support and care.
Medicaid’s Role in Supporting Kids with Special Health Care Needs
For millions of children with disabilities and chronic illnesses, Medicaid is the difference between survival and suffering. Unlike private insurance, which often comes with coverage gaps, high out-of-pocket costs, or exclusions for critical services, Medicaid is designed to cover children’s unique and evolving health care needs and protect families from financial ruin.
1. Medicaid Covers the Services That Private Insurance Won’t
Due to the financial incentives built into private insurance plans, they are frequently built around short-term, acute medical care and not the long-term, specialized services that children with disabilities require. Medicaid fills these critical gaps by covering:
In-home nursing and personal care services: Allowing children with complex medical needs to receive care at home instead of in hospitals or institutions.
Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) benefits: Ensuring early interventions for autism, developmental delays, and chronic conditions before they escalate.
Medical equipment and assistive technology: Providing wheelchairs, ventilators, feeding tubes, and speech-generating devices that children need to move, communicate, and thrive.
Long-term services and supports (LTSS): Helping children remain with their families instead of being placed in institutions.
Specialty care and behavioral health treatment: Providing access to pediatric specialists, therapists, and mental health services that private insurance often excludes or limits.
2. Medicaid Provides Critical Financial Relief for Families
Raising a child with special health care needs is financially overwhelming, even with private insurance. Medicaid ensures that families don’t have to choose between their child’s health and paying their rent, utilities, or grocery bills. Medicaid coverage:
Covers co-pays and deductibles that private insurance only partially funds.
Pays for out-of-network specialists when no local providers are available.
Prevents medical bankruptcy by covering services that would otherwise cost families tens of thousands of dollars out of pocket.
For many families, Medicaid is not a safety net — it’s the only way they can afford life-saving care for their child.
3. Medicaid Supports Caregivers and Keeps Families Together
Caring for a child with disabilities is a full-time job, and Medicaid provides the supports that keep families intact, such as:
Home- and community-based services (HCBS) that allow children to receive care in their homes, surrounded by family, rather than being placed in institutions.
Respite care that gives parents temporary relief from 24/7 caregiving demands, reducing stress and preventing burnout.
School-based health services that provide children with therapies and supports without parents having to miss work for medical appointments.
Without Medicaid, many families would face the heartbreaking decision of placing their child in an institution because they simply cannot provide the level of care needed at home.
The Better Path Forward: Strengthening, Not Slashing, Medicaid for Kids
Instead of rationing care through arbitrary budget caps or limits, policymakers should focus on improving and expanding health coverage for all children. This vision would:
Expand Medicaid/CHIP Eligibility: raising income thresholds and eliminating waiting periods.
Provide for Automatic or Simplified Enrollment: adopting “express lane” enrollment for eligible children to reduce the number of uninsured children.
Increase Medicaid Provider Reimbursement Rates: this provision would help improve access to care and reduce disparities between pediatric care and care provided to adults and senior citizens.
Improve Access to Mental Health Services and Dental Care: addressing the growing youth mental health crisis and the lack of access to oral health.
The Long-Term Benefits of Investing In, and Not Shortchanging, Child Health
Child health coverage is relatively inexpensive in comparison to other populations. Furthermore, investing in children's health through Medicaid not only improves their immediate well-being but also yields substantial long-term economic benefits, such as:
Reduced Mortality and Disability: Early Medicaid coverage has been linked to significant declines in child mortality rates, particularly among non-white children. Additionally, children who received Medicaid benefits have shown reduced disability rates in adulthood, leading to a healthier, more productive workforce.
Increased Employment and Earnings: Access to Medicaid during childhood correlates with higher employment rates and earnings in later life. This suggests that early health interventions enable individuals to contribute more effectively to the economy over their lifetimes.
Government Savings: For each dollar spent on children through Medicaid, the government saves four dollars in future costs, highlighting the program's cost-effectiveness.
Instead of arbitrarily capping and shortchanging Medicaid, we must demand policies that ensure every child gets the care they need to survive and thrive.
Conclusion: The Imperative to Preserve and Strengthen Medicaid
Investing in children's health through Medicaid is both a moral obligation and a sound economic strategy. The program's cost-effectiveness and long-term benefits underscore the importance of maintaining and enhancing Medicaid services for children, especially those with special health care needs. Proposed cuts or caps to Medicaid funding threaten not only the immediate health of millions of children but also the future economic stability and productivity of our nation. It is imperative that policymakers recognize and preserve the invaluable role Medicaid plays in fostering a healthier, more prosperous society.
Call to Action
Contact your members of Congress to express opposition to Medicaid cuts that would harm children. If we don’t stand up for kids, who will?
Share this information with community members, healthcare providers, and advocates to raise awareness about the critical importance of Medicaid for children's health.
Support organizations, including First Focus on Children, that are working to protect and expand Medicaid services for children and families in need.
By taking these steps, we can ensure that Medicaid continues to provide essential health coverage to children with special health care needs, promoting their well-being and contributing to a healthier, more productive future for all.